Early detection of venous disorders: observe visible changes!
VENENCLINIC St. Gallen
9000 St. Gallen
VENENCLINIC Zurich
8004 Zurich
VENENCLINIC Chur
7000 Chur
VENENCLINIC Engadin
7513 Silvaplana

Varicose veins – also known as varicosis – are pathologically dilated and tortuous veins.
Varicose veins represent a sensitive disturbance in the venous drainage of the leg. For reasons of gravity and the increased fatty tissue on the thigh, varicose veins often only appear on the lower leg, although the vein trunk up to the groin or popliteal fossa has no function.
Varicose veins are often caused by defective venous valves in the groin and popliteal region. For this reason, these areas must always be examined and treated if necessary, even if the varicose veins are only visible on the lower leg.
The degeneration of valves can occur anywhere on the leg. Certain risk factors accelerate this process:
Weak connective tissue is a major factor in the development of varicose veins. This is a hereditary predisposition to loose connective tissue, which gives way more quickly under strain. Women are increasingly affected by this, as their hormones have an additional effect on the connective tissue and reduce its firmness. In many young girls, the weakness of the connective tissue is exacerbated by the use of hormone-containing contraceptives.
However, women are also increasingly affected by varicose veins for another reason, namely their pregnancies. Around 30% of all pregnant women suffer from vein problems with their first child and around 50% with their second child, although these often disappear again after the birth. The reason for this is the high pressure exerted by the uterus on the large blood vessels, which makes venous drainage from the leg more difficult.
However, not only pregnancies, but also other factors that increase the pressure in the abdominal cavity can promote the formation of varicose veins. Obesity and chronic constipation can also prevent regular blood drainage.
The amount of exercise plays an important role. A vein needs to be exercised daily, as this is the only way to keep its walls supple and elastic. If the amount of daily exercise decreases, the muscle fibers of the veins atrophy. This is the reason why standing or sedentary occupational groups such as hairdressers, cooks, secretaries, sales assistants etc. often complain of vein problems.
Of course, age also favors the development of varicose veins, as the elasticity of the veins decreases in older people.
Toxins such as alcohol can exacerbate leg problems by having an additional dilating effect on the vein walls.
The term "varicose veins" comes from the Latin varix, which means "twisted" or "swollen vein", describing crooked or tortuous veins. A distinction is made between the following types of varicose veins:
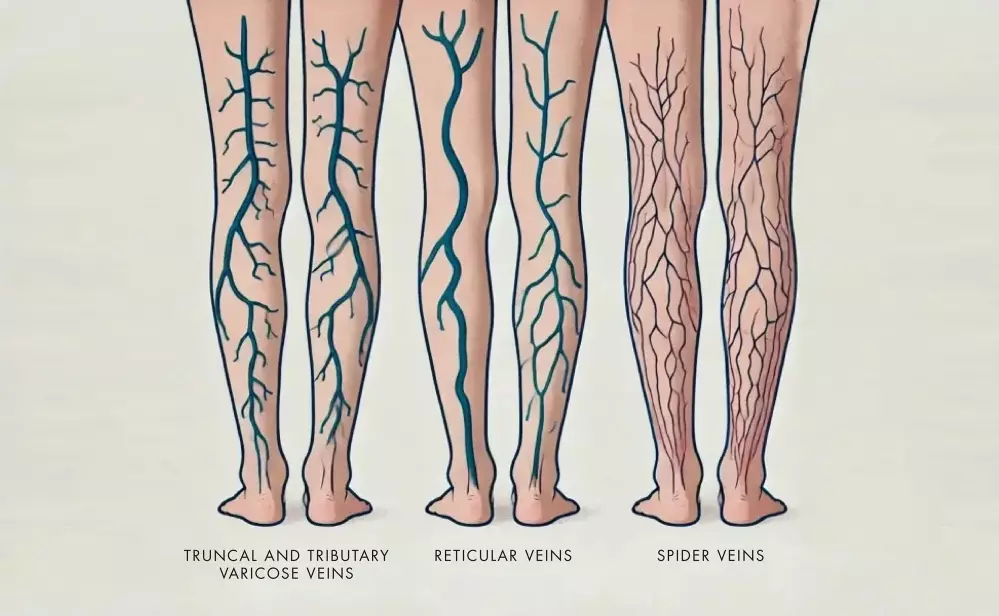
Trunk and side branch varicosis, which is also of the greatest medical importance, occurs in the course of the small and large saphenous veins and their side branches, i.e., on the inside of the leg and on the back of the calf. If someone suffers from trunk and/or side branch varicosis, this is an indication of advanced venous disease, which can lead to a venous leg ulcer if left untreated.
Reticular varicose veins are dilated small veins that lie just under the skin and can occur anywhere on the leg. They have hardly any effect on blood flow. They mainly play a cosmetic role, but it is possible that in individual cases they may cause local discomfort such as itching, pain, etc.
These smallest and finest veins are called spider veins because they resemble the branches of birch twigs that used to be tied into birch twig brooms. The cause of their formation is unclear and their significance is almost exclusively cosmetic.
Reticular varicosis and spider veins can be the first signs and precursors of venous disease.
Varicose veins are not a purely cosmetic problem. Varicosis is a disease that progresses steadily if left untreated and can lead to eczema, venous leg ulcer, thrombosis, inflammation and even bleeding. Varicose veins should therefore not be trivialized and must be examined by a doctor at an early stage. This is the only way to prevent serious consequential damage, from which those affected often have to suffer for the rest of their lives.
Preventing venous leg ulcers is better than treating them, however, which is why it is important to consult a specialist as soon as the first signs of chronic venous insufficiency appear.
Chronic venous diseases are divided into three stages:
Small, bluish dilated skin veins appear, usually around the inner ankle on the lower leg. It is not uncommon for swelling to be accompanied by so-called edema ("water in the legs"), which is particularly noticeable when the shoe no longer fits, or the stocking leaves an imprint in the skin. This first stage itself is not very serious, but can indicate serious venous disease, which is why a careful examination by a leg specialist is advisable.
If the chronic venous disease progresses, the skin begins to turn golden brown, like after a sunburn. It also becomes increasingly thicker, harder and more sensitive to the touch. The whole leg sometimes appears hot, sometimes red and often an agonizing itching sets in. This often develops into eczema. All these signs indicate a serious skin disorder that can soon lead to a venous leg ulcer. At this stage, a specialist must be consulted immediately for clarification and treatment.
In the case of long-standing venous disease, the skin disorder increases as a result of the chronic congestion on the leg to such an extent that even the smallest injuries hardly heal and a venous leg ulcer (ulcus) develops. At this advanced stage, the only thing that helps is consistent compression treatment using bandages followed by a "rubber stocking".
We understand that an aesthetic treatment needs to be carefully considered. We are therefore happy to take the time to answer all your questions during a no-obligation initial consultation. Arrange your consultation appointment at one of our VENENCLINICs today.
If you would like a brief online preliminary clarification before your consultation, you can also contact us by e-mail.
No matter which way you want to contact us - we look forward to hearing/reading from you!